“I had malaria symptoms, so I went to the hospital,” she says, avoiding eye contact. “At the clinic I shared a room with another woman whom I assumed also had malaria. I returned home after I received my medication. But that night I started feeling other symptoms — fever and pain in different parts of my body.”
Nadej was cured from malaria, but she was infected with Ebola from her roommate at the hospital.
“I was not convinced that I had Ebola, or that such a disease even existed,” she says. “I didn’t have an appetite for days; I could have died from starvation. I felt very weak and I spent my day sleeping at home. People around me noticed. Medical teams were inspecting the populations around and when they arrived at my place and I knew I would be hospitalized, I ran away.”
This is DRC’s 10th Ebola outbreak since the disease first appeared in 1976 and has been deemed the most difficult one to manage. The outbreak area is torn by conflicts between armed groups and the country’s official army. On September 22, a deadly clash in Beni resulted in at least 18 deaths. Several armed clashes have followed since. There is also strong resistance from local communities around vaccinations, healthcare inspections, or even believing that Ebola is real.
“I went to the pharmacy to buy medicine the next day. When the pharmacist learned about my symptoms he realized I had Ebola and insisted to take me to the hospital, but I refused,” Nadej says. “I had seen many people in this outbreak go to the hospital and die there. That is what the hospital represented to me: death! I thought if I am going to die anyway, I want to die at home.”
Nadej ran away again, this time to her father’s house in a nearby city. Her father, however, was convinced of Ebola’s existence and its high risk. He recognized his daughter’s symptoms and called the treatment center immediately.
“I was in a very critical condition so I don’t remember how the days passed, but I remember spending two weeks at the hospital,” Nadej says.
She made it out alive and with a better understanding of Ebola, but her return home presented new problems. Her husband, a farmer and the family’s sole provider, abandoned Nadej and their children when he learned of her diagnosis. He’s since remarried.
As is normal practice for any Ebola patient, all her belongings and those of her two babies were incinerated to avoid the risk of contamination. “I returned home from the hospital to an empty house. We had no clothes, all our belongings were burned. How could we survive? I could only think that we could not live anymore.”
Nadej now buys charcoal from the market and sells it outside her residence. It’s not a very populated area, and hardly anyone passes on the dirt path outside her home. “Since my infection, some people have changed their route, thinking that they might be infected by passing near me. To some I’m approachable, to others I should be stigmatized and avoided completely,” she says.
Seven-month-old Mohindo still mainly relies on milk, but Nadej is not allowed to breastfeed him for at least one more year to avoid infecting the baby. With her thin resources, Nadej has to buy two boxes of milk each day for the infant, in addition to their other needs.
“I live thanks to people’s kindness,” she says. “When people pass by and talk to me, I tell them that I had Ebola and that the disease is real. A few people feel sorry for me and help me with a dollar here and there. Each day passes like that and when it ends I wait for the next day in hopes that someone else will visit and help us.”
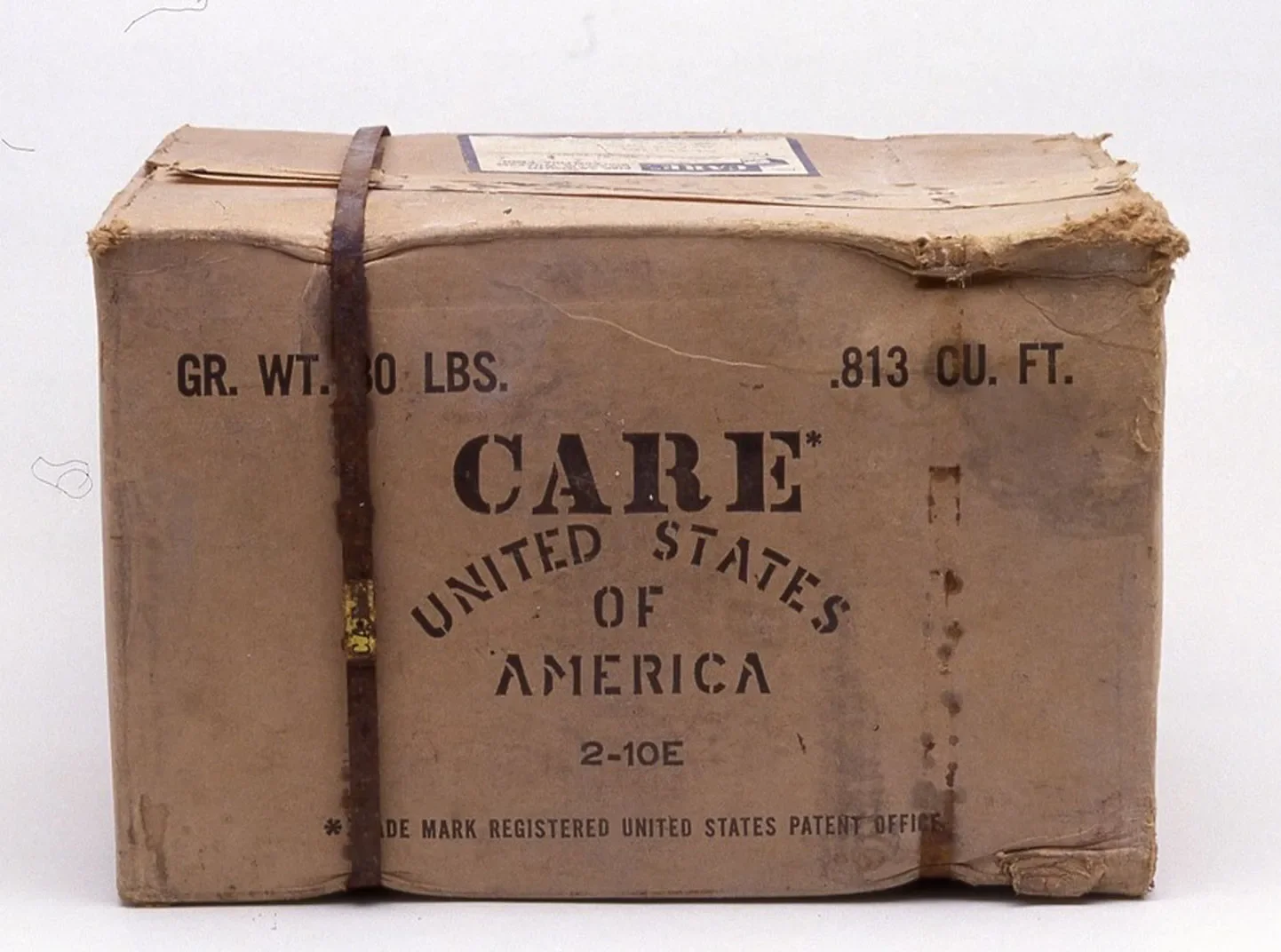
CARE is a member of an inter-agency volunteers’ commission that raises awareness about Ebola, helps reduce stigma, and supports the cured to be reaccepted within their communities, in addition to providing training and hand-washing stations around Ebola-affected cities, and in schools. Some of the cured, like Nadej, also take it on themselves to raise awareness among their communities, even if it results in some backlash.
“Whenever I can, I talk to my community about Ebola.”